Lung cancer is one the most common human malignant diseases. In early disease stages, surgical removal of the tumor represents the treatment of choice. Thereby, excellent long-term success can be achieved by anatomical resection with complete mediastinal lymph node dissection. In many cases, subsequent adjuvant chemotherapy is indicated after successful surgical removal. Ultimatately, in more advanced tumor stages, surgical resection plays also an important role as part of multimodal therapeutic approaches.
Surgical treatment of laryngotracheal diseases is a key focus of the Department of Thoracic Surgery. These often complex procedures are performed in close collaboration with the Department of Phoniatrics and Logopedics (Head: Prof. Dr. Doris-Maria Denk-Linnert).
The most common indications for tracheal surgery are benign stenoses or tumors. Benign airway stenoses typically develop after prolonged intubation or tracheotomy. In contrast, the cause of idiopathic subglottic stenosis—primarily affecting middle-aged women—remains unknown. The resulting airway narrowing severely affects both breathing and voice. Surgical outcomes are excellent, and the operative risk is relatively low. In selected cases, complex resection and reconstruction techniques, including the use of rib cartilage grafts, may be necessary to achieve adequate airway expansion.
Less commonly, tracheal resection is required for malignant disease. In such cases, the goal is complete tumor removal while preserving voice and swallowing function as much as possible.
These procedures are usually performed through a small incision in the neck. In some cases, a partial or full sternotomy, or a lateral thoracic incision (thoracotomy), may be necessary. The department is equipped with specialized ventilation techniques (e.g., high-frequency jet ventilation) and all forms of extracorporeal membrane oxygenation (ECMO) support, which are available as needed for these surgeries.
The surgical spectrum of the laryngotracheal program includes:
- Laryngotracheal reconstruction with cartilage interposition
- Cricotracheal resection
- Tracheal resection (cervical and intrathoracic)
- Emergency management of tracheal injuries
- Carinal resection
- Surgical stabilization for tracheobronchomalacia
- Treatment of tracheoesophageal fistulas
In pediatric cases, the surgical services also include:
- Treatment of long-segment stenoses using slide tracheoplasty
- Correction of congenital airway malformations
- Laryngeal reconstruction with cartilage grafts
Tumors of the mediastinum form a heterogeneous group, which are classified into thymomas, lymphomas, thyroid neoplasms and neurogenic tumors on the basis of the outgoing tissue. In addition to invasive diagnosis by mediastinoscopy, bronchoscopic fine-needle biopsy, or videothoracoscopic evaluation, surgical removal of mediastinal tumors is a domain of thoracic surgery. Even originally benign tumors can otherwise lead to life-threatening complications due to displacing growth. Minimally invasive methods are becoming increasingly important in the surgical field of the mediastinum. In particular, early stage mediastinal tumors are frequently removed at our Department using robot-assisted technology (DaVinci surgical system).
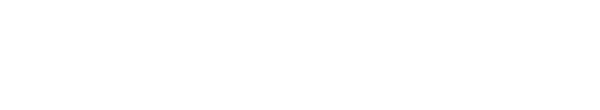
Since tumors of the esophagus are operable only in the limited stages, early detection is of great importance. Esophageal carcinoma is a great challenge for the operating surgeon as the tumor-affected section of the esophagus must be completely removed and then reconstructed. This can be done either by a piece of small intestine, large intestine or by pulling up the stomach.
Malignant pleural mesothelioma (MPM) is an asbestos-associated disease with increasing incidence and high mortality. Despite steady development of diagnostic and therapeutic methods, the prognosis is extraordinarely poor compared to other malignancies.
Treatment options depend on many factors, including stage, location, and infiltration of the tumor, as well as patient age and concomitant diseases.
In recent years, survival advantages have been shown for patients who receive a multimodality treatment strategy - consisting of chemotherapy, surgical resection and radiation therapy.
An established pleural mesothelioma program focusing on diagnostics (video-assisted, minimally invasive thoracoscopy) and radical tumor resection via extrapleural pneumonectomy has emerged at our department in recent years.
Our department is specialized in combination of interventions for tumors crossing organs. In the case of extensive findings with tumorous infiltration of blood vessels, spine, thoracic wall, diaphragm, trachea and esophagus, a multidisciplinary approach is usually required. Often, for tumors that are considered primarily inoperable, curative resection may become possible after induction radiochemotherapy. This requires an individualized approach and patient-specific decision-making.
Resection of lung metastases is one of the most commonly performed thoracic surgical procedures. A variety of tumors preferentially spread to the lungs, such as colorectal carcinoma, renal cell carcinoma, osteosarcoma, soft tissue sarcoma, germ cell tumor, breast carcinoma, and malignant melanoma. Especially in the case of multiple metastatic lesions in the lung, it is important to achieve complete removal of all of these foci. Importantly, the surgical approach is always embedded into an overall oncological concept. The ultimate goal of the surgical approach (pulmonary metastasectomy) is the complete removal of all lung metastases with maximum preservation of lung function. The procedure can usually be performed in a minimally invasive approach (keyhole surgery).
The aim of surgical treatment of pulmonary emphysema is the functional improvement of respiratory mechanics as well as the prophylaxis and treatment of disease-specific complications. Bullectomy involves the selective resection of individual large "bubbles" (= bullae) of the lung. By "Lung Volume Reduction Surgery" (LVRS), larger overinflated areas are removed with the aim of improving the overall respiratory mechanics. LVRS can be performed in appropriate cases using minimally invasive video-assisted surgery (VATS). Furthermore, endobronchial procedures are increasingly used at our department in close cooperation with the clinical department of pulmonology (program director: Univ. Prof. Dr. Daniela Gompelmann).
Our department treats patients with congenital/acquired thoracic wall deformities. The two most common variants are pectus excavatum (funnel chest) and pectus carinatum (keel chest). In addition to aesthetic reasons, the goal of such corrections is to normalize the physiological shape of the chest. This can prevent progression of the deformity and, in extreme cases, secondary damage to the heart.
For pectus deformities, minimally invasive and open corrections are possible depending on the age of the patient. The ideal time window for such surgery is after completion of growth (age: 14-18 years). However, surgical correction is also possible at a later stage (up to the age of 50). In adults (over 18 years) or patients with low thoracic wall elasticity, minimally invasive corrections are technically possible but more painful than open surgery. We therefore recommend a modified open (Ravitch) approach in such cases. Another advantage of Ravitch surgery is that deformities of the costal arch (costal flaring) can also be corrected.
Since 2013, both anterior mediastinum and lung surgeries are performed at our department using the 3rd generation Da-Vinci robot.
In patients with myasthenia gravis, radical thymectomy (removal of the thymus gland) is often indicated. For such operations, the robot is the perfect surgical instrument to remove the entire gland through only three small skin incisions. The robot is also used in the removal of small tumors of the thymus (thymomas). Patients can also benefit from robotic access for lung surgery procedures such as flap removal. Due to the high mobility of the robotic instruments, precise dissection is possible and lymph node removal in particular can be performed optimally.
The cause of CTEPH (chronic thromboembolic pulmonary hypertension) is a buildup of blood clots in the pulmonary arteries. This results in an significant increase in pressure in the pulmonary circulation. The treatment of choice for patients with CTEPH is surgical removal of the thrombotic deposits. This involves peeling off the pulmonary vascular bed on the heart-lung machine under deep hypothermia, in the sense of a true thromboendarterectomy. The results are excellent especially in experienced high-volume centers, where a significant reduction of the pulmonary vascular resistance can be achieved in more than 80% of the cases.
Since 1989, lung transplantation has been one of the main clinical and research focuses of the Department of Thoracic Surgery, where more than 2000 patients have been transplanted to date. Nowadays, the Vienna Lung Transplant Program is one of the five largest lung transplant centers worldwide.
Lung transplantation represents the only therapeutic option for end-stage lung diseases, such as chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, cystic fibrosis or idiopathic pulmonary arterial hypertension. In recent decades, significant advances in perioperative care and long-term follow-up have led to substantial improvements in survival and quality of life.
As a leading center in this field, our department utilizes the most advanced technologies and strategies to provide the best possible medical care. For example, over the past 20 years, various applications of extracorporeal membrane oxygenation have been introduced into our clinical routine, expanding our treatment options. In addition, the continuous development of innovative immunosuppressive options in our center allows us to offer the best personalized treatment options to our patients.
Finally, our department represents one of the leading scientific units. The close collaboration of the research teams with one of the world's most active clinical lung transplant program provides an excellent environment for the translation of newly developed strategies into clinical practice.